We all know that varicose veins are those twisted, enlarged blue veins that tend to bulge from beneath our skin, especially on the back of the leg. They occur when the valves of the veins leak or the walls grow weak. But while most of us can spot a varicose vein or smaller spider vein, there are still a lot of common misconceptions about the condition.
For instance, we often assume that it’s an issue solely for old people or women; but while the chances of developing varicose veins does increase with age, and they are more common in women than in men, the truth is that varicose veins pop up in people of all age groups, both genders and all racial or ethnic backgrounds.
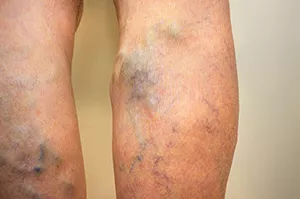
We also tend to dismiss varicose veins as a purely cosmetic issue; but in reality, they can be itchy or painful, cause swelling, increase the risk of blood clots and, in some cases, even develop into ulcers or open wounds. Besides, even if your varicose veins aren’t a health issue, they can make you feel uncomfortable or embarrassed to wear shorts or a swimsuit. Another prevalent myth about varicose veins is that there’s nothing you can do about them. That’s far from true — especially today, as advances in technology and vascular medicine have produced a number of minimally invasive treatments to lessen and eliminate varicose veins.
“The science and methodology are evolving quite rapidly,” says Payam Salehi, MD, PhD, Chief of Vascular Surgery at the CardioVascular Center at Tufts Medical Center. “Older methods like ligation and stripping — as gruesome as it sounds — require general anesthesia and an operating room, and they can lead to bruising and take weeks to heal.”
And with such a full range of new and convenient treatments for varicose veins, people essentially have their choice of which approach is right for them. They can tailor their treatment to their specific conditions and individual needs. There are different types of varicose veins, and patients can experience swelling, discomfort, and even some pain. A primary care physician might start by recommending propping the legs up and using compression. But if that doesn’t fully relieve the pain, patients should be referred to a vascular specialist.
“When there is more than one vein affected, we compare ultrasounds to see where the symptoms are coming from,” said Dr. Salehi. “One vein may be deeper and triggering more pain and discomfort while another vein might be more superficial. Still, both veins could cause significant reflux — when the blood that the veins are supposed to push to the lungs and heart rushes back down into the leg, causing heaviness, discoloration and possibly complications like ulcers.”
But while there are different types of varicose veins, there are also different methods for treating them — each unique to the patient’s situation and lifestyle.
For instance, in the case of a deeper vein, Dr. Salehi sometimes recommends a new low-risk technique called radiofrequency ablation, in which radiofrequency energy heats an area of tissue to the point where scar tissue forms and closes the vein. It requires only tiny incisions on the leg to allow a small catheter inside the problematic vein, and the patient goes home that day to wear a compression stocking for a week or more. Within a month or two, patients often experience a drastic change, feeling little to no debilitating pain. In other cases, there might be spider veins, or varicose veins that are closer to the surface of the skin. In these cases, Dr. Salehi might decide to take a different approach to this vein.
“If the vein we are treating is close to the surface, using heat might burn the skin,” says Dr. Salehi. “So, we might decide on a technique that doesn’t involve heat or a laser.”
One such treatment is sclerotherapy, a minimally invasive procedure in which the doctor injects the vein with a solution that shrinks and collapses the vein, forcing the blood into healthier veins. Afterward, either the doctor removes the varicose vein or it gradually fades from view on its own. These two procedures are just a sampling of all of the convenient, minimally invasive options patients now have to treat their vascular issues. For instance, Tufts Medical Center Vein Center offers these advanced options:
- Non-invasive testing for all types of venous disease
- Radiofrequency and laser ablation of dilated saphenous veins (the primary superficial vein in the inner side of the thigh and calf)
- Sclerotherapy for varicose veins and spider veins
- Laser treatment for spider veins Recanalization and stenting for iliac, subclavian, innominate or vena caval obstruction
- Treatment for perforating veins
- Vein valve transplantation and valve repair for deep venous reflux
- Venous bypass Vena cava filter placement and retrieval
The Tufts MC Vein Center is staffed and directed by doctors who have helped develop some of these treatments. The care team of surgeons, dermatologists, wound care experts and other specialists works side-by-side with patients to make accurate evaluations and plan out the course of treatment that is right for you.
“We always get the newest tech available,” says Dr. Salehi. “We learn about them and test them. If they prove effective, we then adapt them to our practice.”
Dr. Salehi says that he and his team work to ensure the patients are not only physically healthy but that they are also comfortable with the way they feel and look during and after their varicose vein treatment. If you have a varicose vein that is causing symptoms or that you feel you’d like to remove, talk to your physician or contact the Vein Center at Tufts Medical Center. You don’t have to live with varicose veins — no matter what many people might think.
